Clinical Practice Guidelines for diagnosis of amyloidosis: Part 1/3 Year 2020
DOI:
https://doi.org/10.31053/1853.0605.v78.n1.30824Keywords:
amyloidosis, diagnosis, amyloidosis inmunoglobulin light-chain amyloidosis, amyloidosis, familialAbstract
Method: Use the PICO format to generate a series of questions, focusing on the specificity and sensitivity of the amyloidosis diagnostic test. PubMed searches were conducted in English and Spanish from July to August 2019. The level of evidence and recommendation are based on the GRADE system (http://www.gradeworkinggroup.org/index.htm). The recommendations are graded according to their direction (for or against) and strength (strong and weak). Finally, it is recommended to use GLIA tools to evaluate the obstacles and facilitators in implementation.
Suggested explanation: A strong suggestion indicates a high degree of trust in support or opposition to the intervention. When defining a strong recommendation, this guide uses the "recommended" language. The weaker recommendations indicate that the outcome of the intervention (favorable or unfavorable) is doubtful. In this case, if a weak recommendation is defined, the "recommendation" language is used.
How to use these guidelines: Recommendations must be explained within the scope of special care in validated diagnostic studies conducted by specially trained doctors. It is not assumed to change the coexistence conditions of the disease process. Presumably, the attending physician has a high degree of suspicion of amyloidosis. It assumes that diagnostic research is conducted by well-trained doctors using a validated standardized method. This guide is intended for health care professionals and those involved in health care policies to help ensure that the necessary agreements have been reached to provide appropriate care.
Recommendations
For patients with suspected amyloidosis, it is recommended:
- Confirmation in the tissue by biopsy and Congo red staining with the characteristic green birefringence under polarized light is recommended.
- Confirmation by electron microscopy of the biopsy tissue is recommended.
- Protein typing by mass spectrometry is recommended.
- Protein typing by optical and / or electronic immunomicroscopy is recommended, as long as there are reliable antibodies.
- Measurement of serum free light chains is recommended for evaluation of a monoclonal plasma cell proliferative disorder.
- Serum and urinary immunofixation is recommended for evaluation of a monoclonal plasma cell proliferative disorder.
- Measurement of serum free light chains, plus serum and urinary immunofixation is recommended for the evaluation of a monoclonal plasma cell proliferative disorder.
For patients suspected of having amyloidosis, it is suggested:
- Demonstration of a monoclonal plasma cell proliferative disorder by demonstration of clonal plasma cells by the most sensitive technique available in the bone marrow for the diagnosis of AL-type amyloidosis.
- Confirmation of ATTRv amyloidosis by DNA sequencing of the 4-exon amyloidogenic TTR gene in patients with suspected ATTRv amyloidosis.
Downloads
References
Nuvolone M, Merlini G. Systemic amyloidosis: novel therapies and role of biomarkers. Nephrol Dial Transplant. 2017 May 1;32(5):770-780. doi: 10.1093/ndt/gfw305.
Picken MM, Herrera GA, Dogan A. Amyloid and Related Disorders: Surgical Pathology and Clinical Correlations. 2° ed. Humana Press; 2015.
Sipe JD, Benson MD, Buxbaum JN, Ikeda SI, Merlini G, Saraiva MJ, Westermark P. Amyloid fibril proteins and amyloidosis: chemical identification and clinical classification International Society of Amyloidosis 2016 Nomenclature Guidelines. Amyloid. 2016 Dec;23(4):209-213. doi: 10.1080/13506129.2016.1257986.
Benson MD, Buxbaum JN, Eisenberg DS, Merlini G, Saraiva MJM, Sekijima Y, Sipe JD, Westermark P. Amyloid nomenclature 2018: recommendations by the International Society of Amyloidosis (ISA) nomenclature committee. Amyloid. 2018 Dec;25(4):215-219. doi: 10.1080/13506129.2018.1549825.
Hazenberg BP. Amyloidosis: a clinical overview. Rheum Dis Clin North Am. 2013 May;39(2):323-45. doi: 10.1016/j.rdc.2013.02.012.
Aguirre MA, Boietti BR, Nucifora E, Sorroche PB, González Bernaldo de Quirós F, Giunta DH, Posadas-Martínez ML. Incidence rate of amyloidosis in patients from a medical care program in Buenos Aires, Argentina: a prospective cohort. Amyloid. 2016 Sep;23(3):184-187. doi: 10.1080/13506129.2016.1207626.
Merlini G. AL amyloidosis: from molecular mechanisms to targeted therapies. Hematology Am Soc Hematol Educ Program. 2017 Dec 8;2017(1):1-12. doi: 10.1182/asheducation-2017.1.1.
Rowczenio DM, Noor I, Gillmore JD, Lachmann HJ, Whelan C, Hawkins PN, Obici L, Westermark P, Grateau G, Wechalekar AD. Online registry for mutations in hereditary amyloidosis including nomenclature recommendations. Hum Mutat. 2014 Sep;35(9):E2403-12. doi: 10.1002/humu.22619.
Maurer MS, Hanna M, Grogan M, Dispenzieri A, Witteles R, Drachman B, Judge DP, Lenihan DJ, Gottlieb SS, Shah SJ, Steidley DE, Ventura H, Murali S, Silver MA, Jacoby D, Fedson S, Hummel SL, Kristen AV, Damy T, Planté-Bordeneuve V, Coelho T, Mundayat R, Suhr OB, Waddington Cruz M, Rapezzi C; THAOS Investigators. Genotype and Phenotype of Transthyretin Cardiac Amyloidosis: THAOS (Transthyretin Amyloid Outcome Survey). J Am Coll Cardiol. 2016 Jul 12;68(2):161-72. doi: 10.1016/j.jacc.2016.03.596.
Pinney JH, Whelan CJ, Petrie A, Dungu J, Banypersad SM, Sattianayagam P, Wechalekar A, Gibbs SD, Venner CP, Wassef N, McCarthy CA, Gilbertson JA, Rowczenio D, Hawkins PN, Gillmore JD, Lachmann HJ. Senile systemic amyloidosis: clinical features at presentation and outcome. J Am Heart Assoc. 2013 Apr 22;2(2):e000098. doi: 10.1161/JAHA.113.000098.
Gertz MA, Dispenzieri A. Systemic Amyloidosis Recognition, Prognosis, and Therapy: A Systematic Review. JAMA. 2020 Jul 7;324(1):79-89. doi: 10.1001/jama.2020.5493.
Dorbala S, Ando Y, Bokhari S, Dispenzieri A, Falk RH, Ferrari VA, Fontana M, Gheysens O, Gillmore JD, Glaudemans AWJM, Hanna MA, Hazenberg BPC, Kristen AV, Kwong RY, Maurer MS, Merlini G, Miller EJ, Moon JC, Murthy VL, Quarta CC, Rapezzi C, Ruberg FL, Shah SJ, Slart RHJA, Verberne HJ, Bourque JM. ASNC/AHA/ASE/EANM/HFSA/ISA/SCMR/SNMMI expert consensus recommendations for multimodality imaging in cardiac amyloidosis: Part 1 of 2-evidence base and standardized methods of imaging. J Nucl Cardiol. 2019 Dec;26(6):2065-2123. doi: 10.1007/s12350-019-01760-6.
Dorbala S, Ando Y, Bokhari S, Dispenzieri A, Falk RH, Ferrari VA, Fontana M, Gheysens O, Gillmore JD, Glaudemans AWJM, Hanna MA, Hazenberg BPC, Kristen AV, Kwong RY, Maurer MS, Merlini G, Miller EJ, Moon JC, Murthy VL, Quarta CC, Rapezzi C, Ruberg FL, Shah SJ, Slart RHJA, Verberne HJ, Bourque JM. ASNC/AHA/ASE/EANM/HFSA/ISA/SCMR/SNMMI expert consensus recommendations for multimodality imaging in cardiac amyloidosis: Part 2 of 2-Diagnostic criteria and appropriate utilization. J Nucl Cardiol. 2020 Apr;27(2):659-673. doi: 10.1007/s12350-019-01761-5.
Niveles de atención médica y concepto de redes de atención [Internet]. La Salud Como Derecho Social. [consultado el 22 May 2020]. Disponible en: https://sites.google.com/site/lasaludcomoderechosocial/niveles-de-atencion-medica.
Schünemann H, Brożek J, Guyatt G, Oxman A. Manual GRADE para calificar la calidad de la evidencia y la fuerza de la recomendación (1ª Ed. en español). Orrego PA, Rojas MX (Trad.) 2017. Disponible en: http://gdt.guidelinedevelopment.org/app/handbook/handbook.html
Cruz GV. Fernández AR, López FJF. Determinación de prioridades por el Método Hanlon en el laboratorio de análisis clínicos en un hospital de 2do nivel de atención. Waxapa. 2012;1:(6) 80-91.
How we develop NICE guidelines. National Institute for Health and Care Excellence. [consultado 29 Jun 2020]. Disponible en: https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-guidelines/how-we-develop-nice-guidelines
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec 5;5(1):210. doi: 10.1186/s13643-016-0384-4.
Giussani AI, Criniti JM, Malla CG, Manzotti M, Díaz M, Catalano HN. Como se define una recomendación en medicina en base el GRADE (Grading of Recommendations Assessment, Development and Evaluation) Revista Argentina de Medicina. 2014 Sep;2(3): 39–43.
Shiffman RN, Dixon J, Brandt C, Essaihi A, Hsiao A, Michel G, O'Connell R. The GuideLine Implementability Appraisal (GLIA): development of an instrument to identify obstacles to guideline implementation. BMC Med Inform Decis Mak. 2005 Jul 27;5:23. doi: 10.1186/1472-6947-5-23.
GLIA. GuideLine Implementability Appraisal. Yale University. 2005-2011 [consultado 15 May 2020]. Disponible: http://nutmeg.med.yale.edu/glia
Introducción al Manual GRADE. Schünemann H, Brożek J, Guyatt G, Oxman A. Manual GRADE para calificar la calidad de la evidencia y la fuerza de la recomendación (1ª Ed. en español). Orrego PA, Rojas MX (Trad.) 2017. Disponible en: https://gdt.gradepro.org/app/handbook/translations/es/handbook.html#h.2s8eyo1
Adams D, Ando Y, Beirão JM, Coelho T, Gertz MA, Gillmore JD, Hawkins PN, Lousada I, Suhr OB, Merlini G. Expert consensus recommendations to improve diagnosis of ATTR amyloidosis with polyneuropathy. J Neurol. 2020 Jan 6. doi: 10.1007/s00415-019-09688-0.
Maurer MS, Bokhari S, Damy T, Dorbala S, Drachman BM, Fontana M, Grogan M, Kristen AV, Lousada I, Nativi-Nicolau J, Cristina Quarta C, Rapezzi C, Ruberg FL, Witteles R, Merlini G. Expert Consensus Recommendations for the Suspicion and Diagnosis of Transthyretin Cardiac Amyloidosis. Circ Heart Fail. 2019 Sep;12(9):e006075. doi: 10.1161/CIRCHEARTFAILURE.119.006075.
Ando Y, Coelho T, Berk JL, Cruz MW, Ericzon BG, Ikeda S, Lewis WD, Obici L, Planté-Bordeneuve V, Rapezzi C, Said G, Salvi F. Guideline of transthyretin-related hereditary amyloidosis for clinicians. Orphanet J Rare Dis. 2013 Feb 20;8:31. doi: 10.1186/1750-1172-8-31.
Downloads
Published
How to Cite
Issue
Section
License
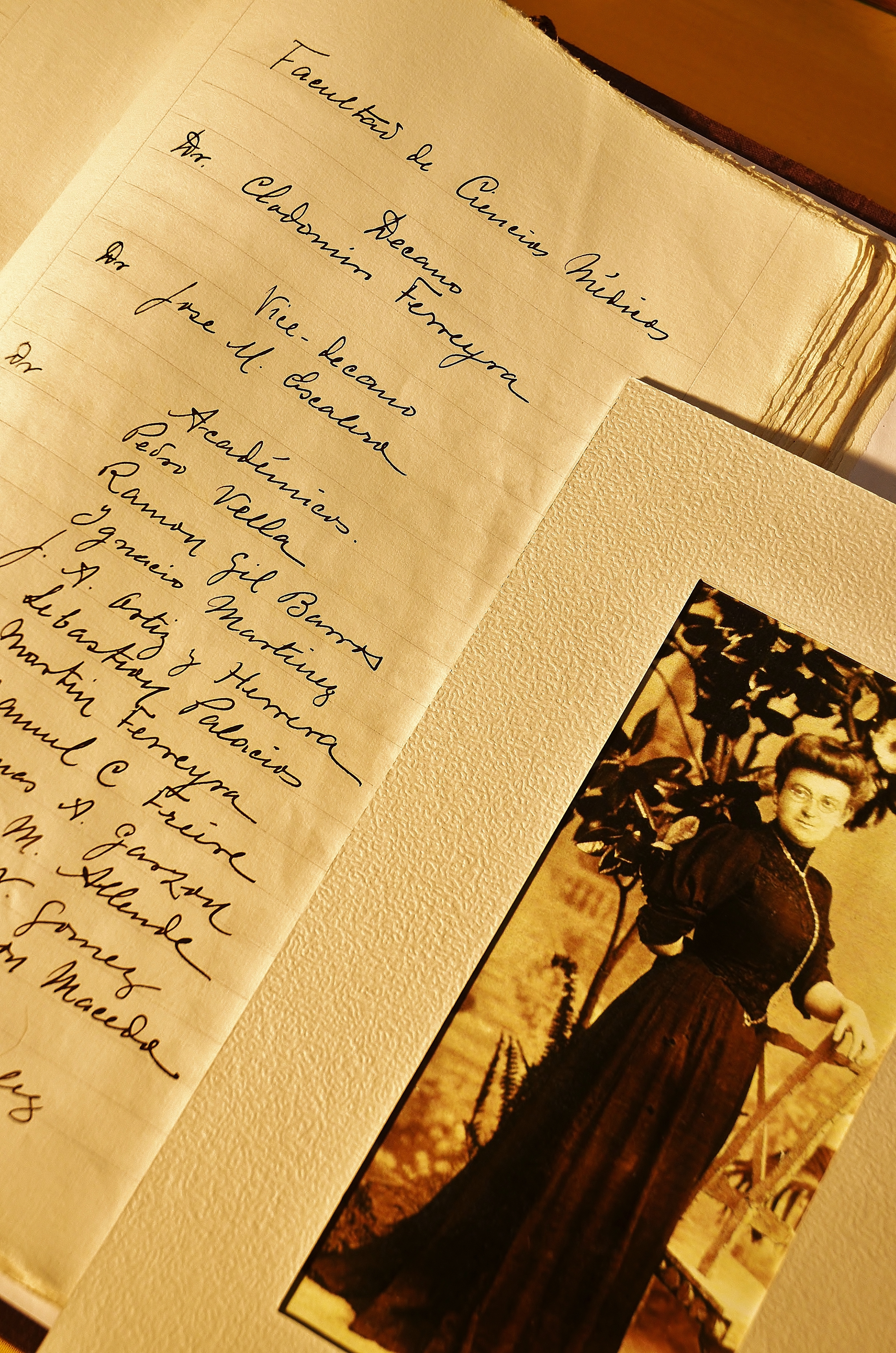
Copyright (c) 2021 Universidad Nacional de Córdoba

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The Faculty of Medical Sciences Journal (RFCM) subscribes to the Open Access policy and does not charge authors fees for publishing, nor does it charge readers fees for accessing published articles (APC).