Metástasis
cerebrales en un paciente con antecedente de mixoma cardíaco: reporte de caso
y revisión de la literatura
Brain metastases in a patient
with antecedent of cardiac myxoma: a Case Report and Review of Literature
Metástases cerebrais em
paciente com antecedente de mixoma cardíaco: relato de caso e revisão de
literatura
Raymundo Solís-Gómez1,2,
Natalia Dávalos-Cabral1,3, Gerardo Arrieta-Limón1,4,
Brandon A. Hurtado-Presa1,5, Andrea Salgado-Alvear1,6,
Laura M. Reyes-Martínez1,7, Fabiola E. Serrano-Arias1,8
DATOS
DE AUTORES
1.
Dirección de enseñanza, Instituto Nacional de Neurología y Neurocirugía
Manuel Velasco Suárez (Ciudad de México, México).
2.
E-mail de contacto: ray.sogo99@gmail.com
ORCID: https://orcid.org/0000-0003-4185-8655
3.
ORCID: https://orcid.org/0009-0001-6340-5123
4.
ORCID: https://orcid.org/0009-0008-3056-4807
5.
ORCID: https://orcid.org/0009-0008-4929-0439
6.
ORCID: https://orcid.org/0000-0002-0232-2578
7.
ORCID: https://orcid.org/0009-0007-8821-0377
8. Clínica de enfermedad vascular cerebral,
Instituto Nacional de Neurología y Neurocirugía Manuel Velasco Suárez (Ciudad
de México, México). ORCID: https://orcid.org/0000-0002-0350-3477
CONCEPTOS
CLAVE
¿Qué
se sabe sobre el tema?
Los
mixomas son una neoplasia cardíaca infrecuente; pueden provocar embolismos por
desprendimiento de un fragmento tumoral, lo que puede ocasionar desarrollo de
metástasis después de años en el sitio de implantación de la porción tumoral
desprendida.
¿Qué
aporta este trabajo?
Existen
pocos casos descritos de metástasis cerebrales secundarios a mixoma cardíaco,
posterior al diagnóstico y resección de la masa tumoral, este reporte de caso
podría contribuir en la discusión de esta rara presentación, en una enfermedad
de baja frecuencia.
Divulgación
Los mixomas son una neoplasia del corazón rara que puede ocasionar
complicaciones como infartos cerebrales y metástasis a lo largo del tiempo.
Estos infartos son ocasionados cuando un fragmento del tumor se desprende y
pasa a circulación sanguínea, a través de la que ocluye vasos sanguíneos cerebrales.
El tratamiento con cirugía cura la enfermedad por el mixoma, sin embargo, no
previene el riesgo de metástasis cerebrales a largo plazo.
Metástasis cerebrales en un paciente con antecedente
de mixoma cardíaco: reporte de caso y revisión de la literatura
Resumen
Introducción. Los mixomas
cardíacos son las neoplasias benignas más comunes del corazón, principalmente
ubicadas en el atrio izquierdo. El tratamiento preferido es la resección del
mixoma. Este método no solo previene complicaciones, sino que también tiene una
baja tasa de recurrencia. Las metástasis cerebrales suelen ocurrir cuando
fragmentos tumorales embolizan e implantan en el lugar de destino. Presentación
del caso. Informamos el caso de un paciente con múltiples metástasis
cerebrales, encontradas durante el seguimiento, después de presentar un
accidente cerebrovascular. Este caso destaca porque la embolización causante de
la metástasis cerebral podría haber ocurrido tanto durante el accidente
cerebrovascular isquémico como durante la remoción del mixoma cardíaco. En
nuestro caso, el paciente fue evaluado durante el seguimiento con resonancia
magnética cerebral, encontrando múltiples lesiones metastásicas. Para
determinar el tipo de lesión, se realizó una biopsia y el diagnóstico histológico
indicativo de tejido metastásico de mixoma atrial izquierdo. Conclusión. Los
pacientes con cardioembolismo deben someterse a un protocolo diagnóstico
completo para distinguir la causa de la embolia, ya sea un coágulo sanguíneo o
un émbolo tumoral. El tratamiento de elección es la resección del mixoma, que
cura los síntomas neurológicos primarios y previene complicaciones
neurológicas. Sin embargo, es esencial mantener una vigilancia activa por más
tiempo para la detección y tratamiento adecuado de metástasis cerebrales.
Palabras clave: neoplasias
encefálicas; metástasis de la neoplasia; neoplasias cardíacas; mixoma;
accidente cerebrovascular embólico
Brain metastases in a patient with antecedent
of cardiac myxoma: a case report and review of literature
Abstract
Introduction. Cardiac myxomas are the most common
benign neoplasms of the heart, mainly located in the left atrium. The preferred
treatment is the resection of the myxoma. This method not only prevents complications
but also has a low recurrence rate. Brain metastases usually occur when tumor
fragments embolize and implant at the destination place. Case presentation. We
report the case of a patient with multiple brain metastases, found during
follow-up, after the presentation of stroke. This case stands out because the
embolization causing the brain metastasis might have occurred either during the
ischemic stroke or when the cardiac myxoma was being removed. In our case, the
patient was evaluated during follow-up with brain magnetic resonance imaging,
finding multiple metastatic lesions. To determine the type of lesion, a biopsy
was performed and the histological diagnosis, which was indicative of
metastatic tissue of left atrial myxoma. Conclusion. Patients with
cardioembolism should undergo a complete diagnostic protocol to distinguish the
cause of embolization, whether it is a blood clot or a tumor embolus. The
treatment of choice is the resection of the myxoma, which cures the primary
neurological symptoms and prevents neurological complications. However, it is
essential to maintain active surveillance for a longer time for the detection
and appropriate treatment of brain metastases.
Keywords: brain
neoplasms; neoplasm metastasis; heart neoplasms; myxoma; embolic stroke
Metástases cerebrais em paciente com antecedente de
mixoma cardíaco: relato de caso e revisão de literatura
Resumo
Introdução. Mixomas cardíacos são
as neoplasias benignas mais comuns do coração, principalmente localizadas no
átrio esquerdo. O tratamento preferido é a ressecção do mixoma. Este método não
apenas previne complicações, mas também tem baixa taxa de recorrência.
Metástases cerebrais geralmente ocorrem quando fragmentos tumorais embolizam e
se implantam no local de destino. Apresentação do caso. Relatamos o caso de um
paciente com múltiplas metástases cerebrais, encontradas durante o
acompanhamento, após apresentar um derrame. Este caso se destaca porque a
embolização causando a metástase cerebral pode ter ocorrido tanto durante o
derrame isquêmico quanto durante a remoção do mixoma cardíaco. Em nosso caso, o
paciente foi avaliado durante o acompanhamento com ressonância magnética
cerebral, encontrando múltiplas lesões metastáticas. Para determinar o tipo de
lesão, foi realizada uma biópsia e o diagnóstico histológico indicativo de
tecido metastático de mixoma atrial esquerdo. Conclusão. Pacientes com
cardioembolismo devem passar por um protocolo diagnóstico completo para
distinguir a causa da embolia, seja um coágulo sanguíneo ou um êmbolo tumoral.
O tratamento de escolha é a ressecção do mixoma, que cura os sintomas
neurológicos primários e previne complicações neurológicas. No entanto, é
essencial manter uma vigilância ativa por mais tempo para a detecção e
tratamento adequado de metástases cerebrais.
Palavras-chave: neoplasias encefálicas; métastase
tumorale; neoplasias cardíacas; mixoma; AVC embólico
Introduction
Myxomas are the most frequent neoplasms
of the heart. 75% of them arise from the left atrium, the most common place of
origin. They develop in adults, at ages between the third and sixth decades of
life, more frequently in women (1). They usually have favorable
outcomes, with a 20-year survival of 85%, and a recurrence rate of less than 5%
(2,3). Complete surgery of the myxoma is the treatment of choice to
cure the disease and prevent neurological complications, however, incomplete
resection of the tumor can result in multifocal tumors and embolism as
recurrence of the disease. The embolization of tumor fragments occurs in about
45% of patients (4). The most frequent site of embolization is the
central nervous system (CNS), leading to neurological manifestations in the
form of stroke, cerebral hemorrhage due to aneurysm formation or cerebral
metastasis due to metastatic deposits of myxoma (3).
Myxomas are benign neoplasms and slow proliferation
lesions. Tumor emboli can remain in any vascular bed and tumor cells can
maintain their viability, forming distant metastases. There have been very few
reported cases of cerebral metastasis, found from 3 months to years after the
diagnosis of myxoma (5). We present the rare case of a patient with
left atrial myxoma with multiple metastatic lesions in the CNS to highlight the
importance of active surveillance for the detection of metastatic lesions and
recurrence of the disease to provide appropriate treatment.
Case
presentation
A 54-year-old woman with no significant medical
history. Five months before her admission, she experienced transient symptoms
of dizziness and decreased strength in her right hand. She went to the
emergency room due to a sudden onset of generalized seizures. The magnetic
resonance imaging showed no lesions (figure
1A). She was protocolized for the history of transient ischemic attack. The
carotid ultrasound showed no atherosclerotic disease. The transthoracic
echocardiogram revealed an intracardiac mass measuring 5.6 x 2.8 cm in size and
a volume of 10 cc, attached to the interatrial septum by a pedicle, mobile, and
protruding into the left ventricle through the anterior mitral valve.
A month later, resection of the intracardiac
tumor was performed with placement of a mitral valve prosthesis and closure of
the patent foramen ovale. The histopathological diagnosis reported a benign
neoplasm of mesenchymal lineage with fusiform and stellar cells grouped
together and forming pseudovascular channels immersed in a
mucopolysaccharide-rich matrix, compatible with myxoma.
Three months
into follow-up, the patient presented with visual field disturbances with left
homonymous hemianopia, seeking evaluation several days after the onset of
symptoms. The simple skull tomography showed a right occipital hypodensity (figure 1B) considered cerebral
ischemia, discharged with medical treatment.

Figure 1. (A) Magnetic resonance imaging without evidence of lesions in the initial
assessment.
(B) Computerized tomography of the skull with right occipital lesion.
The patient
discontinued follow-up, returning three years later due to generalized
seizures. During this hospitalization, brain imaging reported lesions
suggestive of brain metastases in different locations, including the site of the
right occipital infarction (figure 2AB). The histopathological analysis of the
brain biopsy identified neoplastic mesenchymal tissue related to myxoma, with
evidence of old hemorrhage and abundant congestive vessels.
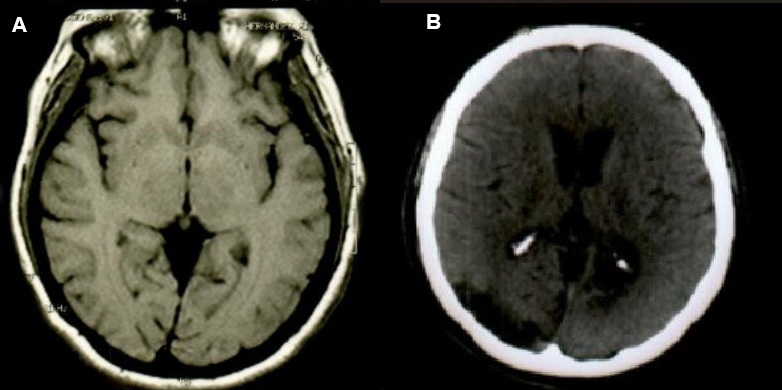
Figure 2AB. Computerized tomography of the skull showing
metastatic lesions involving multiple territories.
Myxomas are the most common benign cardiac tumors, most
of them are sporadic and have slow proliferation. They are thought to derive
from multipotential mesenchymal cells of the endocardium(6).
Embolism phenomena in patients with myxomas occur in
22.4% to 45% of cases, with cerebral embolization in half of the patients who
present it (7,8). Factors associated with a higher risk of embolism
include the external villous appearance, NYHA class (I/II), hypertension,
irregular tumor surface, atypical location, narrow base, and elevated
fibrinogen concentrations (7, 9). The risk of embolism has also been
attributed to blood flow turbulence and the timing of surgical treatment due to
tumor detachment(8,10).
Embolization is due to the detachment of a tumor
fragment from the cardiac myxoma towards the systemic circulation, and the site
of the embolus can be related to the location of the tumor. Right myxomas can
cause pulmonary embolisms, and left ones can cause systemic embolisms that
involve the brain, coronary arteries, or eyes(10), in addition to
being more frequent embolization of left atrial myxomas(8).
Interestingly, at the time of starting the patient's diagnostic protocol, it
was detected that the stroke had a cardioembolic origin. It is thought that
cerebral embolization occurs towards some vessels of the CNS(13),
resulting in cerebral ischemia, infarction, and in some cases, aneurysm
formation(5).
The manifestations of cerebral embolization are three:
ischemic stroke, aneurysms, and cerebral metastases(3,5,10).
Ischemic stroke are mainly due to tumor embolism, causing occlusion of the
cerebral vessels; aneurysms occur due to infiltration of the cerebral vessels
by myxomatous cells through the vasa vasorum, with destruction of their
architecture, weakening of the subintimal tissue, in addition to producing perivascular
injury with subsequent scarring and formation of pseudoaneurysms(10).
Metastases occur due to a transgression of the vessel wall, with focal
alteration of the internal elastic lamina, creating a nest for cerebral
hemorrhage, with the consequent seeding and growth of the tumor tissue in the
cerebral parenchyma(4,11).
In addition to the higher risk of metastasis, related
to overproduction of components involved in myxoma growth, such as CXC or chemotactic
chemokines, endothelin 1 (ET-1), interleukin 8, and growth-related oncogene-α (8,10).
The spectrum of CNS manifestations is broad and
includes progressive headache, nausea, vomiting due to increased intracranial
pressure, weakness or numbness of limbs or body, onset of new seizures, most of
them due to hemorrhage due to aneurysm formation or metastatic space or
occupying lesions(5). In the case presented, loss of control of
urinary sphincters, depressive symptoms, and behavioral alterations were found
in the clinical spectrum when metastatic lesions were found.
Today there is no standard therapy for CNS
complications related to myxoma, resection surgery of the myxoma is the
treatment of choice to prevent additional embolization and neurological complications(4),
in addition to having a good prognosis(5), however, it does not
prevent the risk of cerebral metastases(8), which are presented at
the same time as the myxoma, months or even years after the initial finding of
the cardiac tumor(4,6) or otherwise, before the detection of the
cardiac tumor; in this case, metastatic lesions were detected three years after
the cardiac mass was diagnosed and treated.
A craniotomy is usually performed to resect metastatic
lesions, as in the case we presented. However, successful cases have been
described with lesion remission using gamma knife radiosurgery and temozolomide(3),
the use of chemotherapy with doxorubicin and ifosfamide, with or without
radiotherapy to eliminate proliferating myxomatous cells, could also have
adequate results in case of multiple cerebral metastases to obtain a longer
time without recurrences(6, 12).
The prognosis of myxoma surgical treatment is
generally good, as presented in this case, with almost no postoperative
complications. However, due to the risk of metastasis and recurrence of the
disease, annual follow-up is recommended, at least for more than 3 years and
could even be considered up to eight years later, with the performance of
cerebral magnetic resonance due to the risk of late metastasis(11).
Conclusion
Patients with a cardioembolic event should undergo a complete diagnostic
protocol to distinguish the cause of embolization between a blood clot or a tumor
embolus. This is due to the ability of the myxoma to spread to the brain, which
can result in the development of CNS metastases and the recurrence of long-term
cerebral infarctions.
A standardized treatment has not yet been established, however, myxoma
resection is chosen, with which the primary neurological symptoms are cured,
and neurological complications are prevented. Nevertheless, follow-up up to
eight years later with magnetic resonance imaging for detection of metastases
or over a longer time is essential for the proper treatment of brain
metastases.
1. Saad EA,
Mukherjee T, Gandour G, Fatayerji N, Rammal A, Samuel P, Abdallah N, Ashok T.
Cardiac myxomas: causes, presentations, diagnosis, and management. Ir J Med
Sci. 2024 Apr;193(2):677-688. doi: 10.1007/s11845-023-03531-2.
2. Griborio-Guzman
AG, Aseyev OI, Shah H, Sadreddini M. Cardiac myxomas: clinical presentation,
diagnosis and management. Heart. 2022 May 12;108(11):827-833. doi: 10.1136/heartjnl-2021-319479.
3. Ma K, Zhao D,
Li X, Duan H, Yan C, Wang S, Zeng L, Xu K, Lai Y, Chen B, Mu N, Yang C, Quan Y,
Li Z, Wang X, Feng H, Li F. Case report: Multiple brain metastases of atrial
myxoma: Clinical experience and literature review. Front Neurol. 2023 Feb
8;13:1046441. doi: 10.3389/fneur.2022.1046441.
4. Rajeshwari M, Subramanian P, Suri
V, Nambirajan A, Garg A, Vibha D, Phalak M, Sharma MC. Metastatic
lesions of atrial myxoma. A pathologist can clinch them all. Neuropathology.
2020 Jun;40(3):295-301. doi: 10.1111/neup.12640.
5. Rodrigues D,
Matthews N, Scoones D, Aziz F, Nath F. Recurrent cerebral metastasis from a
cardiac myxoma: case report and review of literature. Br J Neurosurg. 2006
Oct;20(5):318-20. doi: 10.1080/02688690601000394.
6. Wan Y, Du H,
Zhang L, Guo S, Xu L, Li Y, He H, Zhou L, Chen Y, Mao L, Jin H, Hu B. Multiple
cerebral metastases and metastatic aneurysms in patients with left atrial
Myxoma: a case report. BMC Neurol. 2019 Oct 23;19(1):249. doi:
10.1186/s12883-019-1474-4.
7. Liu Y, Wang J,
Guo L, Ping L. Risk factors of embolism for the cardiac myxoma patients: a
systematic review and metanalysis. BMC Cardiovasc Disord. 2020 Jul
25;20(1):348. doi: 10.1186/s12872-020-01631-w.
8. Rose D, Papa A,
Tomao S, Greco E, Zacharias J. Cerebral Metastases in Patients with Left Atrial
Myxoma. J Card Surg. 2016 May;31(5):289-93. doi: 10.1111/jocs.12727.
9. Amemiya K,
Yonemoto Y, Ishibashi-Ueda H, Matsumoto M, Ohta-Ogo K, Ikeda Y, Kobayashi J,
Fukushima S, Fujita T, Hatakeyama K. Morphological characteristics of cardiac
myxoma causing embolism: a series of 40 years of experience at a single
institute. Virchows Arch. 2023 Feb;482(2):377-384. doi:
10.1007/s00428-022-03461-x.
10. Niño AO, Ramirez LAC, Leal JCA,
Ortiz SM, Cordoba LG. Brain manifestations secondary to auricular myxoma. Radiol
Case Rep. 2020 Sep 17;15(11):2371-2374. doi: 10.1016/j.radcr.2020.08.043.
11. Ghodasara SA, Balasubramanian R,
Varadharajan S, Shobhanaa PS. Cardiac phoenix in the brain-occult intracranial
hemorrhagic metastases from completely resected atrial myxoma. Surg Neurol Int.
2020 Nov 11;11:383. doi: 10.25259/SNI_410_2020.
12. Bernet F, Stulz
PM, Carrel TP. Long-term remission after resection, chemotherapy, and
irradiation of a metastatic myxoma. Ann Thorac Surg. 1998 Nov;66(5):1791-2.
doi: 10.1016/s0003-4975(98)00917-5.
Conflicto
de interés:
Ninguno.
Limitaciones
de responsabilidad
La
responsabilidad de esta publicación es de los autores.
Fuentes
de apoyo
La
presente investigación no contó con fuentes de apoyo.
Originalidad
Este artículo es original y no ha
sido enviado para su publicación a otro medio de difusión científica en forma
completa ni parcialmente.
Cesión de derechos
Quienes participaron en la
elaboración de este artículo, ceden los derechos de autor a la Universidad
Nacional de Córdoba para publicar en la Revista de la Facultad de Ciencias
Médicas de Córdoba y realizar las traducciones necesarias al idioma inglés.
Contribución de los autores
Quienes participaron en la
elaboración de este artículo, han trabajado en la concepción del diseño,
recolección de la información y elaboración del manuscrito, haciéndose
públicamente responsables de su contenido y aprobando su versión final.
Recibido: 2024-04-05 Aceptado: 2024-08-27
 https://creativecommons.org/licenses/by-nc/4.0/
https://creativecommons.org/licenses/by-nc/4.0/
 DOI: http://dx.doi.org/ 10.31053/1853.0605.v81.n4.44662
DOI: http://dx.doi.org/ 10.31053/1853.0605.v81.n4.44662
©Universidad Nacional de Córdoba